Diseases We Treat
Angiology and vascular surgery is a medical specialty that studies and treats circulatory diseases. It is a medical-surgical specialty, meaning it treats diseases with both medication and surgery when the patient needs it.

All diseases affecting the veins and arteries, except for the arteries of the heart and cranial arteries, which are treated by cardiologists and neurosurgeons, respectively.
The most frequent diseases are: Venous, Varicose veins in all their degrees, venous thromboembolic disease which includes (deep vein thrombosis, pulmonary thromboembolism and post-thrombotic syndrome), varicose ulcers, venous injuries due to weapons, due to surgical complications, hemangiomas and venous malformations.
Angiology and Vascular Surgery
- What diseases does an angiologist and vascular surgeon treat?
- What does an angiologist and vascular surgeon treat?
Arterial Diseases: Chronic arterial insufficiency, acute arterial insufficiency, arterial thromboembolism, arterial aneurysms, aorta and peripheral arteries, vasospastic diseases such as Raynaud's disease, Buerger's disease, etc. Arterial injuries due to weapons, or surgical complications, carotid body tumor (glomus or paragangliomas), carotid disease.
Other diseases: Diabetic foot, chronic wounds, lymphedema.
Patients with kidney failure who require vascular access for hemodialysis, such as an arteriovenous fistula or central venous catheter placement; patients with cancer who require central venous access, such as a reservoir catheter for chemotherapy.
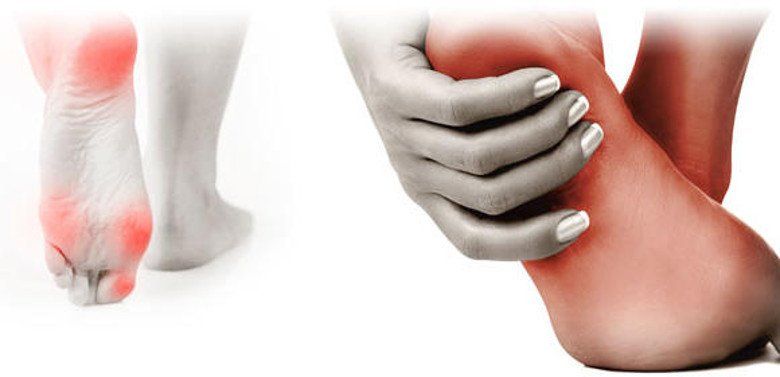
Diabetic foot is a devastating complication of diabetes mellitus, caused by nerve degeneration, occlusion of blood vessels associated with infection, and gangrene.

Diabetes mellitus is the leading cause of lower limb loss. Eighty percent of amputations begin with an unnoticed injury, and in most cases, they could have been avoided. If you have diabetes and suffer a foot injury, time is of the essence. Seek treatment as soon as possible to avoid fatal complications.
Diabetic foot
To treat any foot injury in patients with diabetes, the first step is to ensure circulation. If circulation is lacking, any treatment is unsuccessful. Before undergoing amputation, all patients with diabetes should be evaluated by an angiologist and vascular surgeon.
• Pain or fatigue when walking.
• Changes in skin color or temperature.
• Dryness.
• Ulcers.
• Calluses on the sole of the foot.
• Areas of low sensitivity.
• Immobility in the joints.
• Changes in walking or balance.
• Cuts, scrapes, blisters, or anything that affects the integrity of the foot.
• Ingrown, thick, infected nails, etc.
Veins are the blood vessels that carry blood back to the heart after nourishing the body's organs. From the heart, it travels to the lungs to be oxygenated and sent back to the entire body.

This cycle, which repeats itself incessantly, must overcome various obstacles (especially the blood returning from the feet to the heart). The first obstacle is the force of gravity, and the second is hydrostatic pressure (i.e., the blood from below must push the blood from above). For this blood return to occur properly, the venous wall and valves must be intact. When any of these mechanisms fail, blood returns to the heart with difficulty and can stagnate in the veins, causing dilation, tortuosity (a serpentine appearance of the veins), edema, or swelling.
Chronic Venous Disease or Varicose Veins
In its early stages, it only has cosmetic repercussions with the appearance of varicose veins, creating an unsightly appearance on the legs. Later, pain, cramps, heaviness, and fatigue may appear, and in its advanced stages, complications such as lipodermatosclerosis (hardened and blotchy skin), bleeding (varicorrhage), clot formation (varicothrombosis), and ulcers can be disabling, also affecting the patient's family, social, and emotional life. This condition is commonly known as chronic venous disease, varicose vein syndrome, or varicose veins. Its causes include: Predisposing factors: Heredity and deep vein thrombosis. Triggering factors: Prolonged standing or sitting motionless, multiple pregnancies, blows or injuries, high doses of female hormones (estrogens), flat feet, and exposure to high temperatures.
Aggravating factors: Obesity, sedentary lifestyle and diabetes.
Laser varicose vein surgery
Currently, more than 90% of varicose veins can be removed in the vast majority of patients who suffer from them. Request an evaluation with us and we will help you resolve your problem.
What are the causes and symptoms of thrombosis?
For blood to fulfill its function, it must remain liquid, and for this to happen, there must be a balance between procoagulant and anticoagulant factors. When this balance is disturbed, thrombosis (thrombophilia) or, conversely, hemorrhage (hemophilia) can occur.
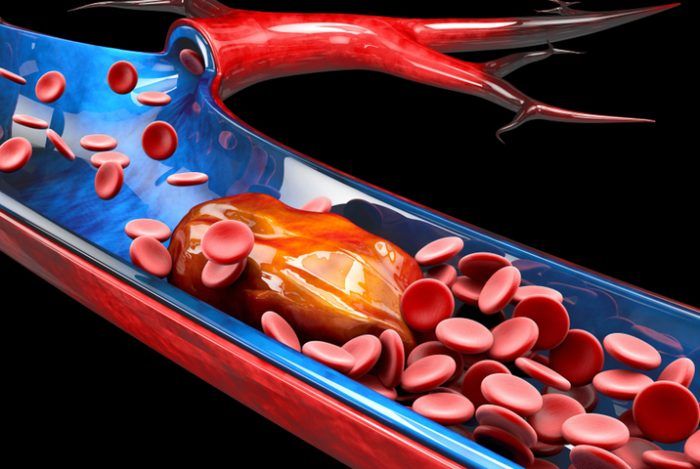
90% of DVT cases occur in the lower extremities, most frequently on the left, and the signs and symptoms are:
Pain, increased volume, increased circumference in the affected limb, color change at the site of thrombosis, and edema.
Deep Vein Thrombosis
We are all at risk for thrombosis, but if you have one or more of the following conditions, your risk increases:
*History of thrombosis in the family.
*Antecedente de trombofilia en la familia.
*Suffer from any collagen disease (Rheumatoid arthritis, Scleroderma, Lupus, among others).
*Pregnancy (not all pregnant women experience it).
*Suffer from cancer.
*Obesity.
*Age over 40 years (Under certain circumstances).
*Orthopedic surgery (Hip or knee).
*Long trips (more than 4 hours or more than 5,000 km) by any means of transport. (Economy Class Syndrome).
*Prolonged prostration (spending a lot of time in bed).
*Multiple fractures.
*Immobilization (Use of splint or cast).
*Central venous catheter.
*If you use oral contraceptives or hormone replacement therapy.
*If you have already suffered from thrombosis, you may experience it again.
Diabetic neuropathy
Diabetic neuropathy is a type of nerve damage that can occur if you have diabetes. High blood glucose can damage nerves throughout the body. Diabetic neuropathy most commonly affects the nerves in the legs and feet.
Depending on which nerves are affected, symptoms of diabetic neuropathy include pain and numbness in the legs, feet, and hands. It can also cause problems with the digestive system, urinary tract, blood vessels, and heart. For some people, symptoms are mild. However, in other cases, diabetic neuropathy can be quite painful and disabling.
Peripheral neuropathy
This type of neuropathy may also be called distal symmetric peripheral neuropathy. It is the most common type of diabetic neuropathy. It first affects the feet and legs, followed by the hands and arms. Signs and symptoms of peripheral neuropathy typically worsen at night. These include:
- Numbness and reduced ability to feel pain or perceive temperature changes
- Tingling or burning sensation
- Cramps or stabbing pains
- Muscle weakness
- Extreme sensitivity to touch (for some people, even contact with bed sheets can be painful)
- Serious foot problems, such as ulcers, infections, and damage to bones and joints
When should you consult a doctor?
Call your healthcare provider to make an appointment if:
- You have a cut or sore on your foot that is infected or does not heal
- You have burning, tingling, weakness, or pain in your hands or feet that interferes with your daily activities or sleep
- You notice changes in digestion, urination, or sexual activity
- You experience dizziness and fainting
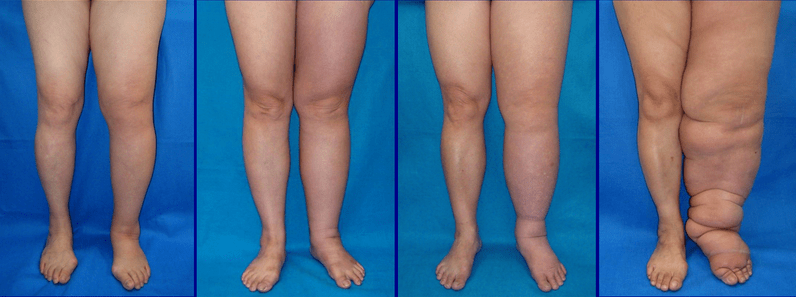
Signs and symptoms of lymphedema include:
- Swelling of all or part of the arm or leg, including the toes and fingers
- Feeling of heaviness or oppression
- Limited range of motion
- Recurrent infections
- Hardening and thickening of the skin (fibrosis)
When you should see a doctor
Make an appointment with your doctor if you notice persistent swelling in your arms or legs. If you've already been diagnosed with lymphedema, see your doctor if there is a sudden and dramatic increase in the size of the affected limb.
Lymphedema
Complications
Complications of lymphedema may include:
- Skin infections (cellulitis). Trapped fluid creates a breeding ground for germs, and even a minor injury to the arm or leg can be an entry point for infection. The affected skin appears swollen and red, and is often painful to the touch and feels warm. Your doctor may prescribe antibiotics so you can have them on hand and start taking them immediately.
- Sepsis. Untreated cellulitis can spread to the bloodstream and trigger sepsis, a life-threatening condition that occurs when the body's response to an infection causes damage to its own tissues. Sepsis requires emergency medical treatment.
- Drainage through the skin. With severe swelling, lymphatic fluid may drain through small breaks in the skin or cause blisters.
- Skin changes. In some people with very severe lymphedema, the skin on the affected limb may thicken and harden, taking on the appearance of elephant skin.
- Cancer. A rare form of soft tissue cancer can develop as a result of more severe cases of lymphedema that go untreated.
Vascular Access for Hemodialysis
Dialysis and hemodialysis
Dialysis is used to treat end-stage renal failure. This procedure removes waste products from the blood when the kidneys can no longer perform their job.
There are different types of kidney dialysis. This clinic focuses on hemodialysis.
What is a vascular access?
A vascular access is an opening made in the skin and blood vessel during a short operation. When you have dialysis, your blood flows through the opening into the hemodialysis machine. Once your blood has been filtered in the machine, it flows back through the access into your body.
What is hemodialysis?
The main function of your kidneys is to remove toxins and excess fluid from your blood. If these waste products accumulate in your body, it can be dangerous and even lead to death.
Hemodialysis can:
- Eliminate extra salt, water, and waste products so they don't build up in your body
- Maintain safe levels of minerals and vitamins in your body
- Help control blood pressure
- Help produce red blood cells
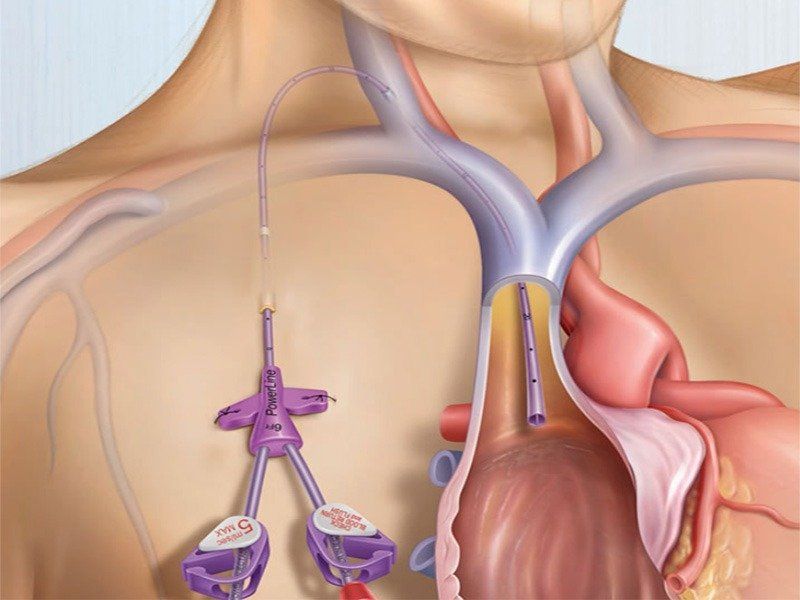
When to call the doctor
- Bleeding from the vascular access site
- Signs of infection, such as redness, swelling, pain, tenderness, warmth, or pus around the site
- A fever of more than 100.3°F (38.0°C)
- The flow (thrill) in the graft or fistula decreases or is not felt at all
- The arm where the catheter was placed swells and the hand on that side feels cold.
- Your hand becomes cold, numb, or weak
Risks and complications
As with any procedure, peripheral vascular intervention involves certain risks and complications, which may include:
- Allergic reaction to contrast medium.
- Bleeding or infection at the puncture site
- Recurrent narrowing of the artery.
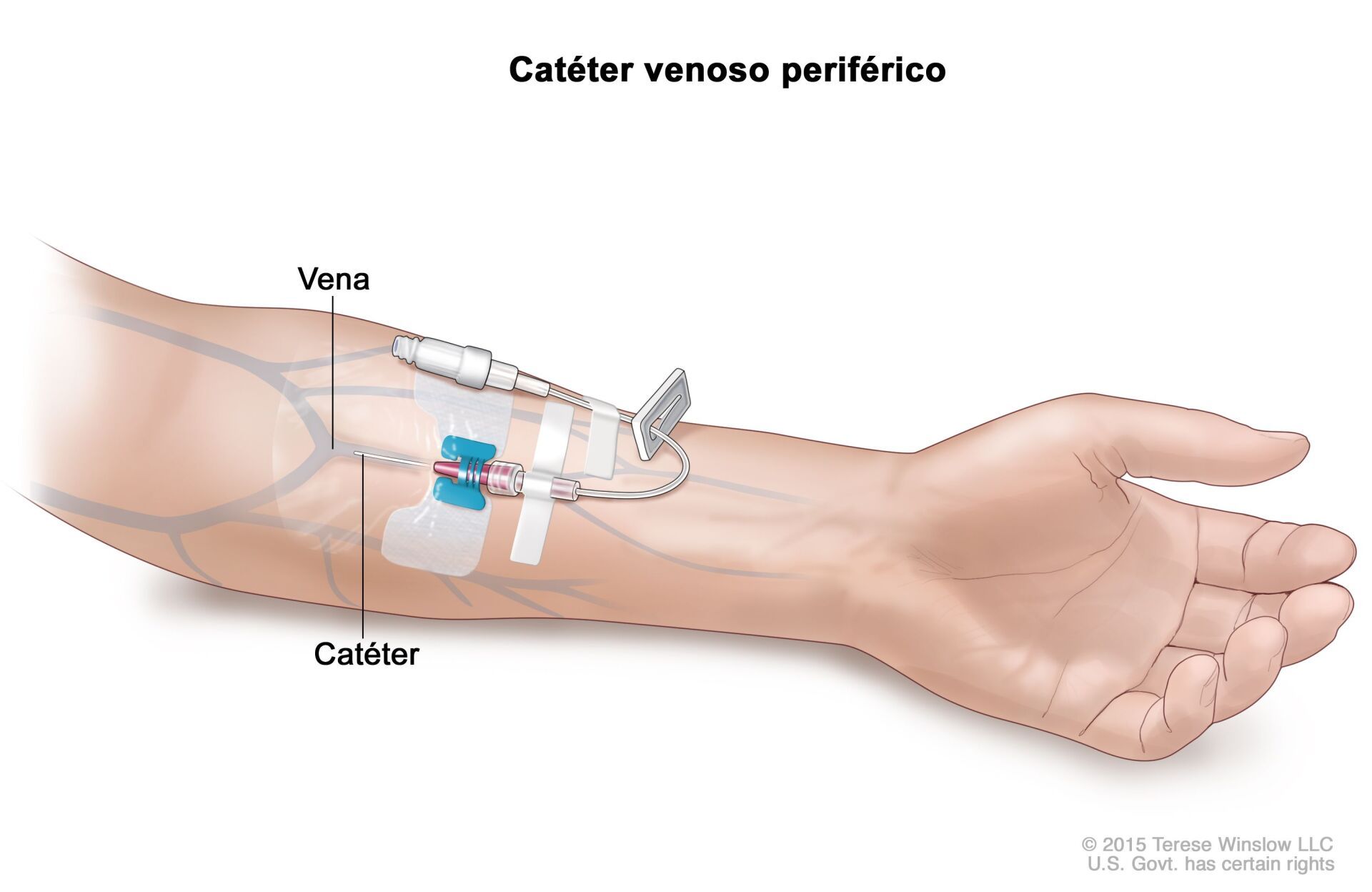
Peripheral Vascular Catheterization
When patients suffer from hardening of the arteries, or atherosclerosis, their arteries are partially blocked by a substance called plaque. When these blockages occur in the legs or arms, they are called peripheral artery disease.
In most patients, intravenous fluid and medication needs can be met with a percutaneous peripheral venous catheter. If blind percutaneous placement is difficult, ultrasound guidance usually achieves successful insertion. Rarely, a venous view may be used when percutaneous catheter insertion is not feasible. Typical venous cannulation sites are the cephalic vein in the arm and the saphenous vein in the ankle. However, venous clamping is rarely necessary due to the widespread use of peripherally inserted central catheters (PICCs) and intraosseous lines in adults and children.
Cardiovascular diseases are the third cause of death in Mexico.
Among the most common conditions are chronic venous disease known as varicose veins, varicose ulcers, deep vein thrombosis, chronic arterial insufficiency, acute arterial insufficiency, and diabetic foot.